Innovative Solution For Liver Diagnosis

Innovative Solution For Liver Diagnosis
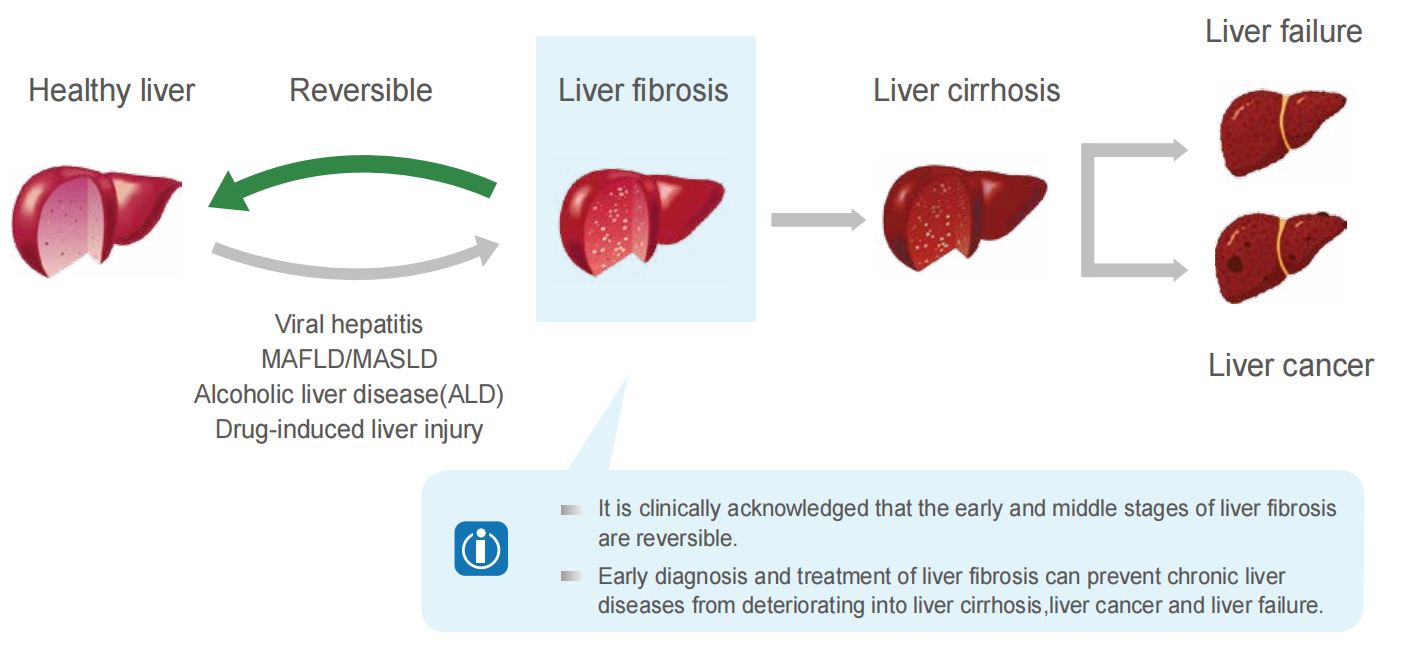
Liver Health Killer: Liver Fibrosis
Liver fibrosis is the common pathological process in various chronic liver diseases leading to liver cirrhosis
Early detection is key to slowing the progression of liver disease
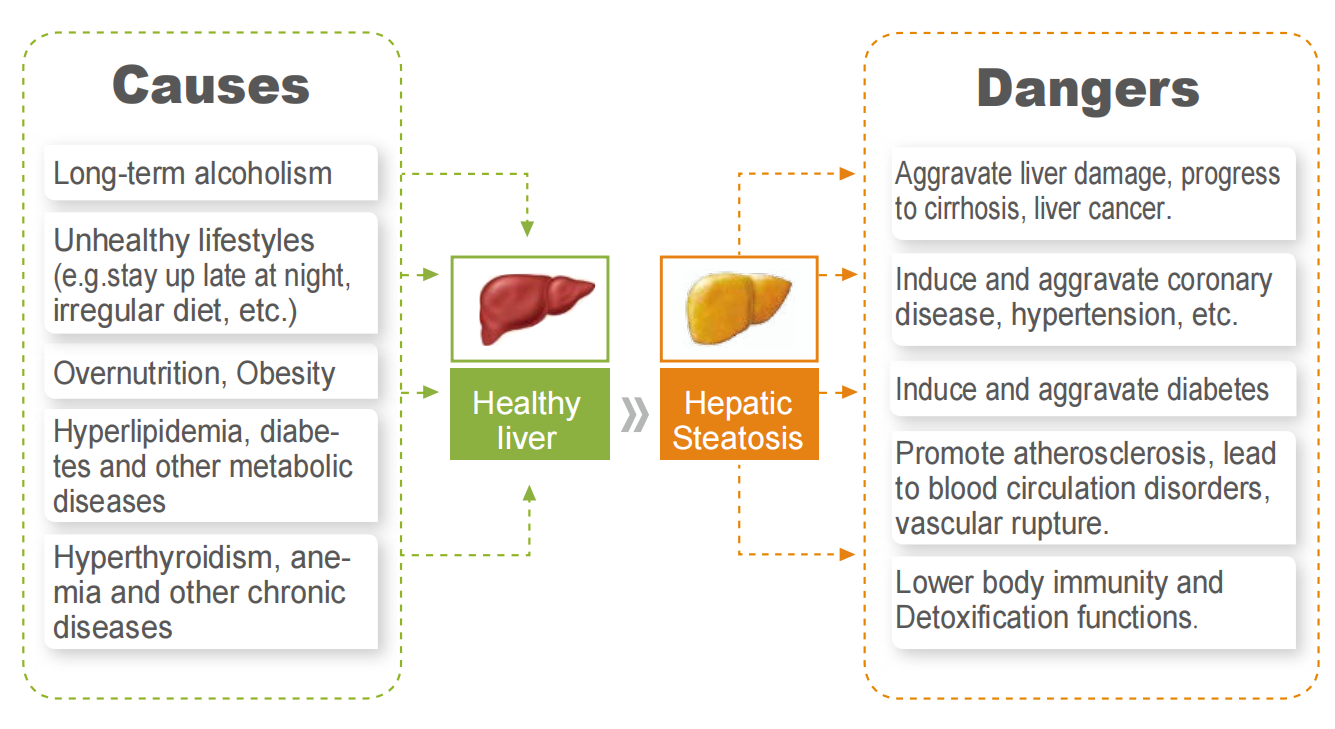
Liver Health Killer: Hepatic Steatosis
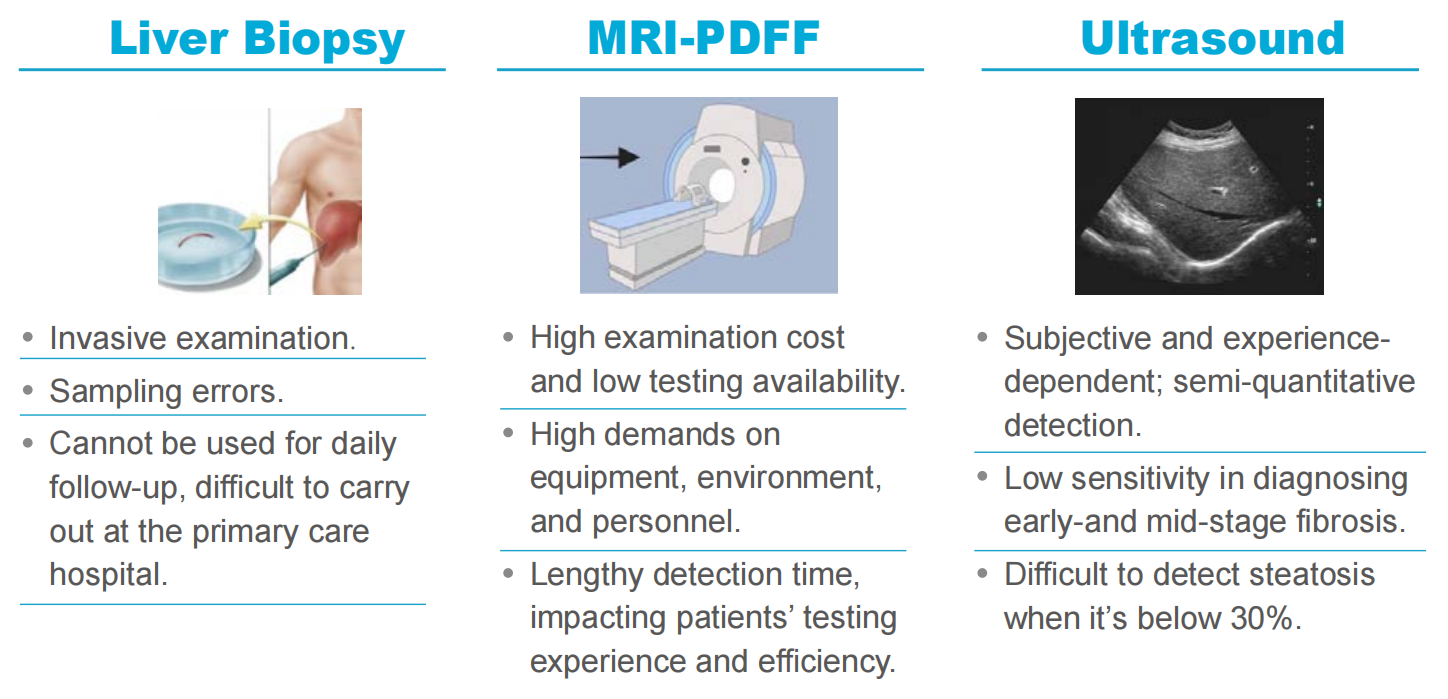
Challenges in Existing Diagnostic Methods
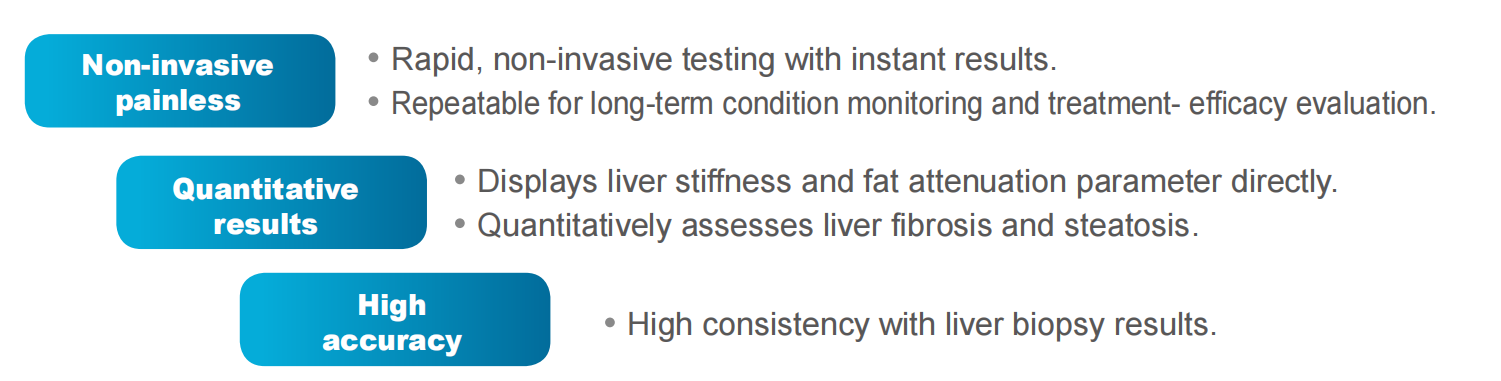
LivTouch® Advatages
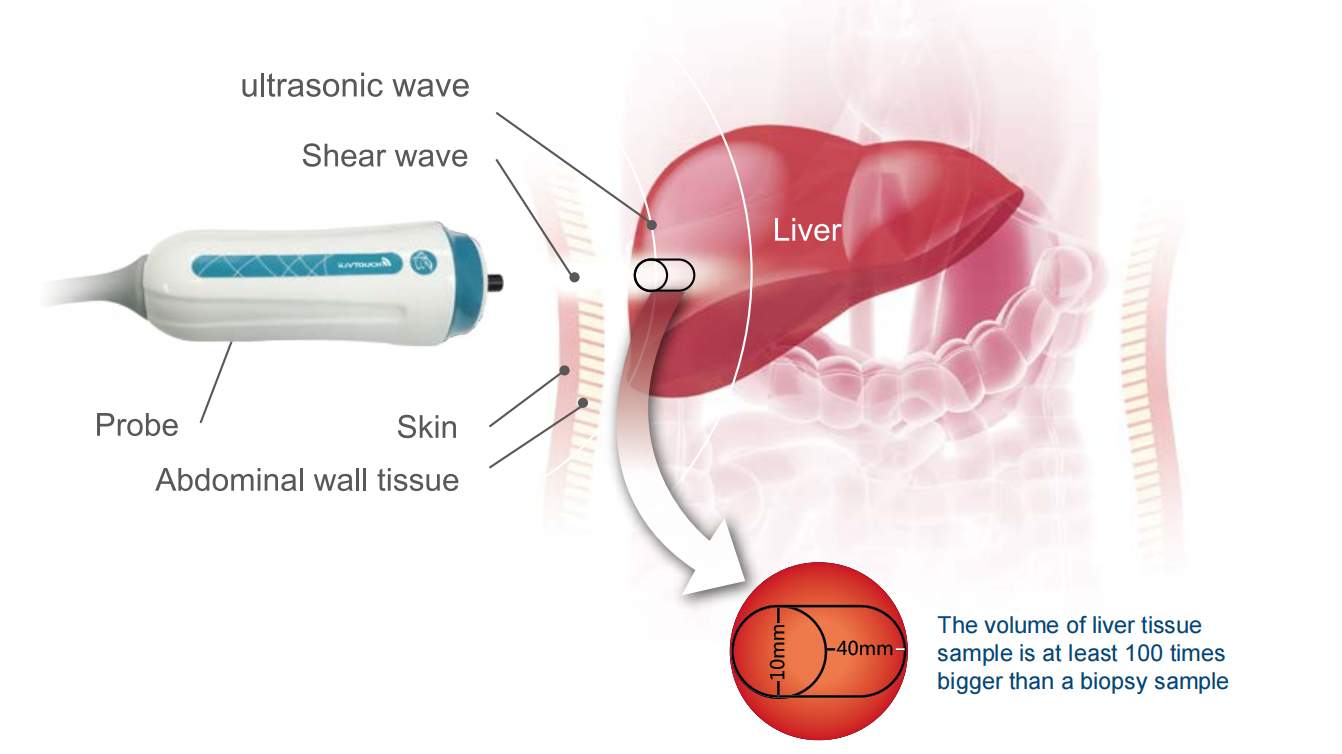
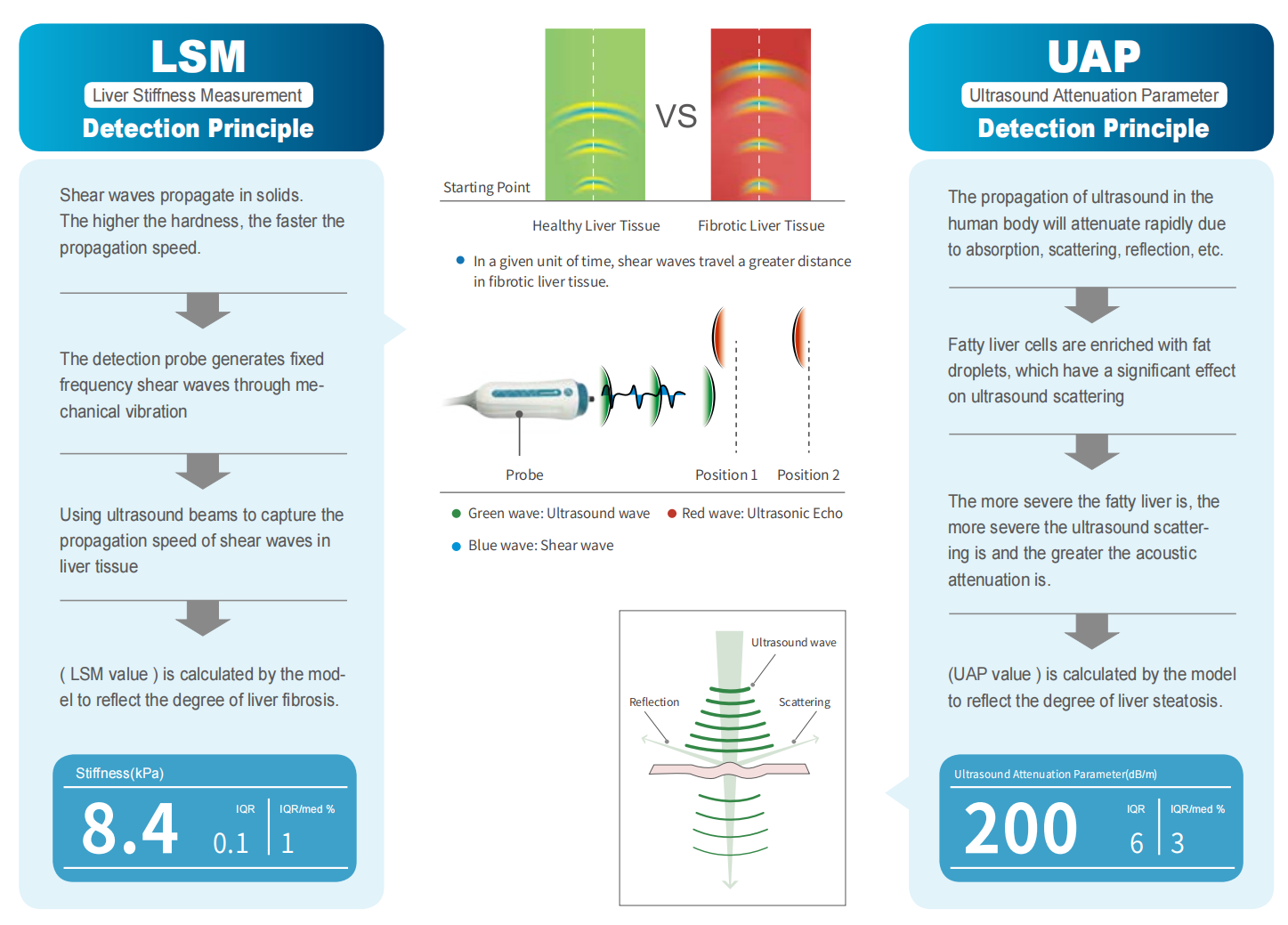
iLivTouch®: Precise detection for liver fibrosis and steatosis